Overcoming Infertility
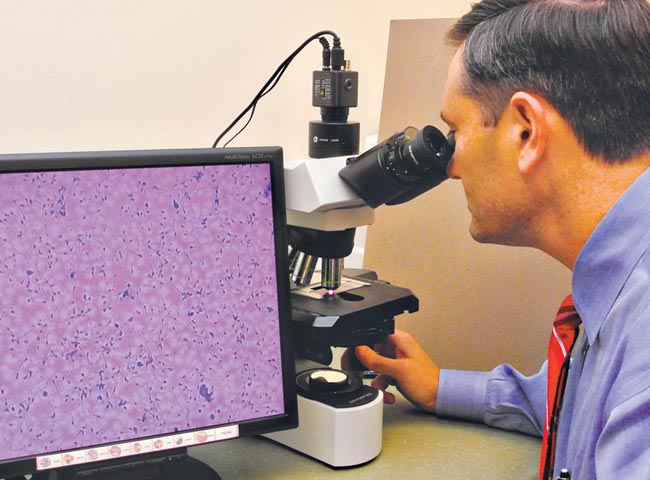
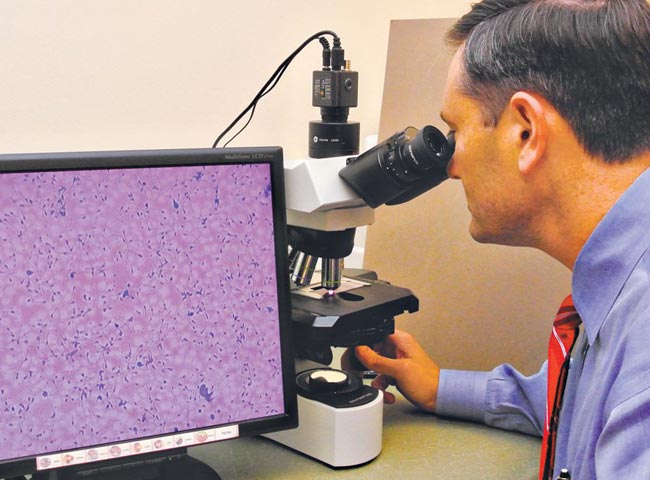
John L. Frattarelli, founder and director at the Fertility Institute of Hawaii
Where did you receive your schooling and training?
I did my undergraduate at Vanderbilt University in Nashville, Tenn.; medical school at the University of Tennessee in Memphis; residency for OB/GYN at Walter Reed Army Medical Center in Washington, D.C.; and fellowship in reproductive endocrinology and infertility at the National Institutes of Health in Maryland.
How long have you been practicing?
I finished my fellowship in 2000. I had a military obligation for medical school, so I was sent to Tripler. I started the Fertility Institute of Hawaii in 2008.
At what point should a couple come in for help with fertility?
Immediately – if there is a known fertility problem.
In general, 80 percent of couples who do not have fertility issues will conceive within the first six months of trying.
How do you determine what the problem is?
For men, it’s fairly easy.
We have them give us a sperm sample, and we do a thorough analysis of that sample to evaluate the quantity, motility and quality of the sperm as well as several other traits. The whole function of sperm is to get into the egg. That’s what we’re assessing when we evaluate sperm: Can the sperm get into the egg or not? If not, what can we do to help?
For a woman, it’s much more complex. We’re not only looking to see what’s maybe preventing her from getting pregnant, but ultimately we want to make sure she has a safe, healthy pregnancy without an increased risk of miscarrying. We check to make sure the fallopian tubes are open, that the uterus is normal and the uterine cavity where the baby would grow is normal. We also confirm that the reproductive hormone levels are appropriate for producing an egg, ovulating and carrying the pregnancy safely.
How do you help?
First, we are able to offer every possible fertility therapy. Most diagnoses can be treated with medical therapy, surgical therapy or one of the numerous in vitro fertilization (IVF) therapies. Therapies have improved and changed over the years. Ten to 20 years ago patients would receive surgery if their tubes were blocked, but tubes don’t respond well to an insult. Once they get damaged, it’s almost impossible to fix them. If a patient has fallopian tube blockage or damage, nowadays surgery is not recommended and IVF is recommended.
Surgery is often an option for patients who have a uterine problem, like a fibroid or polyp in the cavity of the uterus. Uterine abnormalities are likely to cause miscarriages and can be diagnosed by ultrasound. We also evaluate hormone levels. If there’s a hormonal imbalance, medications can be used that will often help a woman ovulate (produce an egg).
For men, if there’s a sperm problem, there are really only a couple of treatment options. Medications rarely will help sperm abnormalities. Instead, procedures like IVF or intrauterine inseminations are used. During an intrauterine insemination we place sperm directly into the uterus. We place approximately 20 times more sperm into the uterus than what gets into the uterus with intercourse. By increasing the sheer number of sperm when we know that a woman is ovulating, the chances of pregnancy are greatly improved. If the sperm is really abnormal, the only other option is to do IVF but also do a special technique ICSI (intra-cytoplasmic sperm injection), where we take one sperm and directly insert it into the egg.
The sperm doesn’t have to do anything, it just has to be there and we do all the work. With IVF and ICSI, you almost take the man out of the equation. As long as there’s sperm, it doesn’t have to be moving and the fertility mostly falls on the ability of getting a good egg.
Does IVF therapy often result in twins/triplets?
It’s not necessarily the insemination part – putting the sperm into the uterus – that leads to multiples, it’s how many eggs are available. Giving women injectable or oral medications can lead to multiple follicles being developed, and that can lead to multiples. We try very diligently to prevent multiples. Obviously there’s a higher risk for the mother and the baby if someone has multiples. The risk is increased drastically for triplets and more.
What are the latest technological advances in the field?
One of the great things about this field is that there are exciting new technologies being developed to help patients all the time. One of the things we’ve been able to do recently is freeze eggs. As a field, we have been trying to freeze eggs for years, but the problem is that until recently we didn’t have the right technology to freeze eggs well. With the successes of a recent technology called vitrification, we are now able to freeze eggs with the same fidelity that we freeze sperm and embryos. For fertility preservation, we can now take a patient who wants to dedicate time to her career early in life and freeze her eggs.
Later, she can try to get pregnant (at the age of 38 or later) when she may have had difficulty using her eggs at that age.
Along these same lines, we’ve recently developed a donor egg bank. A donor egg bank is like a sperm bank, but with eggs. We now have donor eggs for patients who need them, such as older patients whose own eggs aren’t viable or can’t produce a viable pregnancy. Now, instead of doing a fresh donor cycle, which is very costly and time consuming and sometimes difficult to synchronize, with the egg bank patients can come in and we can cycle them up right away. They can do a cycle with donor eggs and have excellent pregnancy rates for less than half the cost of a fresh egg cycle.