International Stroke Forum
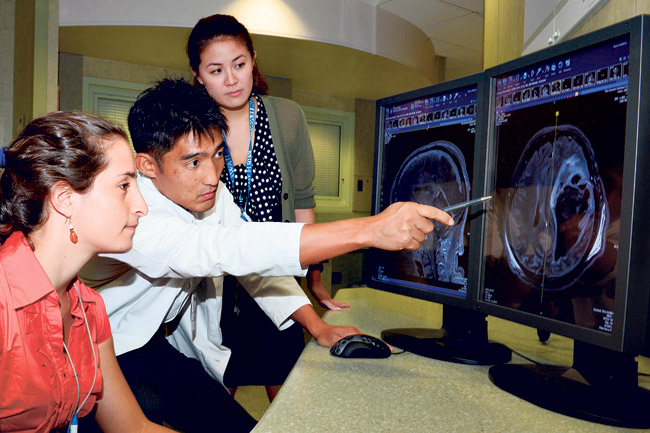
Dr. Kazuma Nakagawa
Neurointensivist and vascular neurologist at The Queen’s Medical Center
Where did you receive your schooling/training?
I went to Cornell University for my undergraduate studies and University of Florida College of Medicine for my graduate medical studies. I did my internship and neurology residency at Harvard, and neurocritical care/neurovascular fellowship at University of California at San Francisco.
dih_2
How long have you been practicing?
I’ve been practicing at Queen’s for a little more than two years. I am also assistant professor of medicine at the University of Hawaii John A. Burns School of Medicine.
What is an ischemic stroke?
Ischemic stroke occurs when a blood clot blocks an artery supplying oxygenated blood to an area of the brain. When this part of the brain stops getting blood flow, it can cause permanent brain damage.
What is a hemorrhagic stroke?
Hemorrhagic stroke occurs when an artery in the brain breaks, causing bleeding into that region of the brain, and mechanical and, at times, permanent damage to the brain.
Are strokes preventable?
Yes, up to 80 percent of strokes are preventable. The major controllable risk factors that people can work on are high blood pressure, diabetes, high cholesterol, arrythmia and other heart conditions, obesity, smoking and physical inactivity. Most of these can be controlled with a healthier lifestyle, routine medical visits and being on the appropriate medications. By controlling these risk factors, one can significantly reduce the risk of having an ischemic or hemorrhagic stroke in his or her lifetime.
What demographic is most affected by strokes?
Recent evidence suggests that the burden of both ischemic and hemorrhagic strokes is not borne equally by all, with racial minority groups reported to have a higher burden of stroke risk factors and younger age of stroke onset compared to Caucasians.
Are there findings particular to the population here in Hawaii?
Until recently, most stroke studies that looked at racial disparities have focused on African-Americans and Mexican-Americans, and there was no major stroke-related research on our Native Hawaiian and Pacific Islander population. In 2010, my research team began looking at stroke disparities among our local population. Over the past two years, we’ve published two major papers showing a major disparity among Native Hawaiians and other Pacific Islanders in Hawaii with strokes.
Our first major finding is that Native Hawaiians and other Pacific Islanders who were hospitalized with hemorrhagic stroke were significantly younger, by more than 10 years, and had higher prevalence of diabetes and hypertension compared to Caucasians.
Our second major finding is that Native Hawaiians and other Pacific Islanders who were hospitalized with ischemic stroke also were significantly younger, by more than 10 years, and had higher prevalence of diabetes, high blood pressure and obesity compared to Caucasians.
Are Native Hawaiians and Pacific Islanders often underrepresented in studies?
Yes. One of the major problems is that Native Hawaiians and other Pacific Islanders have been historically aggregated with Asians into a single racial/ethnic category in many clinical studies, which may have masked differences that may, at times, be substantial.
What causes the disparities seen in this population?
To be honest, I don’t exactly know the main factor that is driving the stroke disparities seen in this population. This issue is very complex since reasons for health disparities involve both biological and social factors that can affect the disease process. Although I do think that genetics may play some role here, much of the disparities also can be attributed to the complex effect of the social environment.
Our team is currently conducting a prospective cohort study called “Queen Emma Stroke Study” to better understand the main factor that is driving stroke-related disparities seen in our local population. We also are investigating if there is any difference in the long-term outcome after stroke among different racial/ethnic groups. I named the research project in honor of our hospital founder, Queen Emma, who had the vision to deliver excellent health care equally to everyone in Hawaii. Our long-term goal is to conduct a culturally sensitive, community-based intervention study that can improve stroke-related outcomes and reduce health disparities among Native Hawaiians/Pacific Islanders and other underserved minorities living in Hawaii.
You will be presenting at the International Stroke Conference at the Hawaii Convention Center, Feb. 6-8.
The International Stroke Conference is one of the largest annual conferences for clinicians and researchers around the world who specialize in the field of stroke and other cardiovascular diseases. This is where some of the newest and cutting-edge research findings are presented for the first time. Special symposia, debates and abstract presentations will focus on numerous topics that are relevant to patient care that may potentially change how we practice every day. Although this conference has been around for many years, this is the first time it is being held in Honolulu.
I will be presenting two abstracts at the conference. One will describe the effect of methamphetamine abuse on the young age of hemorrhagic stroke among our local population. Our other abstract will describe the possible gender differences in the preference of endof-life care by the patient after a hemorrhagic stroke. To my knowledge, neither of these topics has been published or presented elsewhere.